✿ General Principles
☞ Definitions
- UTI is a bacterial infection that affects parts of the urinary tract.
★Anatomic [解剖學] - 細菌是尿道口往上進入逆尿系統,故我們也由下往上看!!
► lower: urethritis, prostatitis, cystitis (superficial infection of bladder)
▪ Urethritis [尿道炎]: often sexually-transmitted
▪ Cystitis [膀胱炎]: traditional UTI
▪ Prostatitis [前列腺炎]: in men (廢話 XD)
▪ Prostatitis [前列腺炎]: in men (廢話 XD)
► upper; pyelonephritis [腎盂腎炎]
★Clinical
complicated [合併併發症]: in women, any UTI men or pregnant women with underlying disease
✿ Clinical manifestations
▲Cystitis: dysuria [解尿疼痛], urgency [急尿], frequency [頻尿], burning sensation [解尿灼熱感], hematuria [血尿], 改變尿液的顏色和氣味, suprapubic [恥骨部]疼痛; 一般不會發燒
▲Urethritis: 除了有尿道分泌物外,其餘症狀與 cystitis 一樣. cystitis 和 urethritis 都應排除 viginitis [陰道炎]的症狀
▲Prostatitis:
chronic: 除了有排尿困難 (hesitancy [解尿遲疑], weak stream [尿流慢])外,其餘其餘症狀與 cystitis 一樣
acute: perineal [會陰部]疼痛, fever, 有 tenderness [壓痛]的 prostate [攝護腺]
▲Pyelonephritis: fever, chills [畏寒], flank [腹側] or back pain, 噁心, 嘔吐, 腹瀉
▲Renal abscess
▲Renal abscess
► Urinalysis [尿液檢查]: pyuria [膿尿] + bacteriuria [菌尿症] ± hematuria ± nitrites
我們總是在書上看到 UTI 會有以上這4種現象,但卻沒告訴我們其臨床意義,那就趁現在好好了解一下吧~
我們總是在書上看到 UTI 會有以上這4種現象,但卻沒告訴我們其臨床意義,那就趁現在好好了解一下吧~
♣ Urine Routine;Urinalysis [尿液常規]
▪ WBC [白血球]: 尿中的白血球通常以嗜中性球為主,淋巴球次之,而是酸性性最少。
→ 輔助診斷各種腎臟疾病
→ 尿液中出現過多的嗜中性球 (高倍視野下超過5顆):又稱為 pyuria, 表示泌尿道出現感染或發炎。
▪ Bacteria [細菌]: 正常情形下,尿液中不該出現細菌,當尿中發現有細菌時,表示有 UTI 可能,但須排除不正確收集尿液方式所造成的外陰部細菌汙染。
→ 輔助診斷 UTI
→ 尿液中發現有細菌: 表示有 bacteriuria
▪ Occult Blood [潛血]: 當有大量血尿、血紅素尿或肌紅蛋白尿時,尿液通常呈現紅色或棕色,此時可用尿液潛血試驗來鑑別其他造成紅棕色尿液的原因。
→ 篩檢 hematuria [血尿]、hemoglobinuria [血紅素尿]、myoglobinuria [肌紅蛋白]
→ hematuria: 指尿中出現紅血球
▪ RBC [紅血球]: 正常情況下,尿中 RBC 在高倍視野下不超過2顆。
▪ Nitrite [亞硝酸鹽]: 許多細菌,泌尿道感染時,例如 Escherichia coli [大腸桿菌], Klebsiella [克雷白氏菌], Enterobacter [腸桿菌], Proteus [變形桿菌], Staphylococcus [葡萄球菌], Pseudomonasa [假單孢菌]可將尿液中的 nitrate [硝酸鹽]代謝成 nitrite [亞硝酸鹽], 當尿中細菌大於 10^5/mL 時, nitrite 大量產生便會呈現陽性反應。
→ 診斷 UTI 的間接方法
→ Nitrite (+): UTI
→ Enterococcus, Neisseria gonorrhea 及 Mycobacterium tuberculosis 不會將 nitrate 代謝成 nitrite.
▪ Leukocyte Esterase [白血球酯酶]: 尿液中若存在有大量嗜中性球即暗示有 UTI, 嗜中性球會釋放出 esterase, 故尿中 leukocyte esterase 增加為診斷 UTI 的間接方法。因尿液中嗜中性球並不穩定而容易分解,當顯微鏡檢尿液沉渣未發現大量白血球,而病患又有 UTI症狀時, leukocyte esterase 便可當作輔助診斷的工具。
→ 診斷 UTI 的間接方法
→ Leukocyte Esterase (+): 懷疑有 pyuria
► Urine Cx : 當有 symptoms 時才需做 cx (culture).
→ 從 clean-catch midstream [清潔排出之中段尿液] or straight-cath specimen [導尿管檢體]
▪ Significant bacterial counts:
typically ≧10^5 CFU/mL in women, ≧10^3 CFU/mL in men or cathrterized [導尿] Pts.
▪ Pyuria & (-) UCx = sterile pyuria [無菌性膿尿症]
→ urethritis, nephritis [腎炎], renal tuberculosis [腎結核感染], foreign body [異物]
► Blood culture: 有 febrile Pts 才需要; 考慮有 complicated UTIs
✿ Microbiology
▪ Uncomplicated UTI: E.oli (80%), Proteus, Klebsiella, S. saprophyticus
→ 在健康的人和非懷孕婦女: lactobacilli, enterococci, Group B strep and coag-neg staph (except S. saprophyticus) 通常是汙染物
▪ Complicated UTI: E.coli (30%), enterococci (20%), PsA (20%), S. epi (15%), other GNR
▪ Catheter-associated UTI: yeast (30%), E.Coli, other GNR, enterococci, S. epi
▪ Urethritis: Chlamydia trachomatis, Neisseria gonorrhoeae, Ureaplasma urealyticum, Trichomonas vaginalis, Mycoplasma genitalium, HSV
Referance:
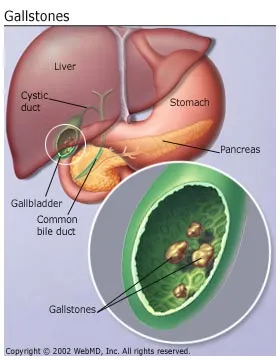
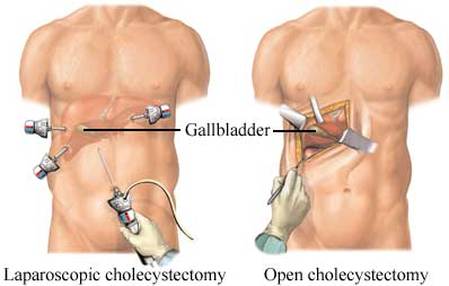
- The Washington Manual of Medical Therapeutics 34th Edition, Pancreatobiliary Disorders.Gallstone Disease
- The Massachuetts General Hospital Handbook of Internal Medicine 5th Edition, Urinary Tract Infections